In his annual letter to shareholders this past weekend, Warren Buffett referred to a portion of Berkshire Hathway’s money as “cost free.” He previously has referred to some of Berkshire’s cash as “free money” so this is nothing new.
That “free money” — which I will explain in a moment is not really free, hence the title of this post — is from the insurance businesses that Berkshire owns.
As a brief ‘splainer if you don’t want to Google “Warren Buffett Free Money Insurance:” The insurance biz makes money two ways. The first is by taking your premiums and then years later paying out claims. If the underwriters are doing their jobs well, an insurance business will take in for example, $100 in premiums and pay out $90 in claims and operating costs.
This is a great business, because unlike making widgets where you have to first spend for the raw materials before making and selling the widget, with insurance premiums you actually get the revenue up front and pay later.
Which brings us to the second part of the insurance business, which Buffett calls the “free” part. What happens to those premiums in the interim? Known as the float, that money gets invested. And if you are a conglomerate like Berkshire, you have plenty of businesses to invest in.
So even if an insurer’s underwriters fail at their jobs, and they pay out $105 in costs and claims for each $100 in premiums, they still may have profited with an additional $30 or more in “free” money that was invested in the intervening years.
As Buffett explained in 2019:
If our premiums exceed the total of our expenses and eventual losses, our insurance operation registers an underwriting profit that adds to the investment income the float produces. When such a profit is earned, we enjoy the use of free money – and, better yet, get paid for holding it.
How much they actually make all depends on how long they can invest that float. Delay, delay, delay is, therefore, sometimes in the best interests of the insurance company.
But as I said, the money isn’t free. It has a cost. And that cost is borne by the people that lost their homes to a fire, flood or hurricane (BH owns property insurers), or were injured in car collisions (BH owns Geico), or injured due to medical malpractice (BH owns MLMIC) .
If a claim is delayed because of bad faith on the part of the insurer, the claimant effectively becomes the banker for Berkshire Hathaway. Buffett gets to keep using money to which the claimants are entitled. For free.
A brief example from one of my own cases so you can see it in practice, but any personal injury attorney can relate similar ones:
Simple car collision. Easy liability. Significant injuries. The injured can’t work. The insurance coverage is only $100K. Geico offers $4K eight months after the collision. Hey, maybe the injured is desperate and Geico won’t need to even pay the claim? Five months later they are big sports and increase the offer to $5K. Eighteen months after initial offer they are $12.5K.
Without dragging the whole story out, it takes Geico almost 3 ½ years from its first offer to tender its $100K policy (and over four years from date of collision). Free money? For Berkshire, yes. They were able to invest the money the whole time. But that is money that should have been in the hands of the injured claimant.
Given that Berkshire as a whole has had average annual returns of 20% since 1965, it’s easy to see how the use of that money can pile up — for Berkshire. But not for the injured person that has to lean on friends and relatives to get by.
The problem, here in New York, is that we don’t have a statute that explicitly deals with bad faith insurance tactics. Other states do. Just not New York.
To pursue a bad faith claim in an auto case for example, one must first take a verdict in excess of the insurance policy (years after the injury has taken place) and then the insured person against whom that excess verdict was taken (previously known as the defendant) can sue their own insurance carrier.
But the people who were actually injured can’t do it. They have to hope that the insured will get on board with this. And if the insured is judgment-proof, they may just walk away and say tough noogies.
New York, it should be clear, needs bad faith legislation to prevent this abuse — which will stop insurance companies from using bad faith tactics to stall the payment of claims.
The pandemic has made things worse, with extensive backlogs in the courthouse. As I noted in 2021, a year into the pandemic, if we had a decent bad faith statute many of these delays would vanish.
Even Alabama handles bath faith claims better than us.
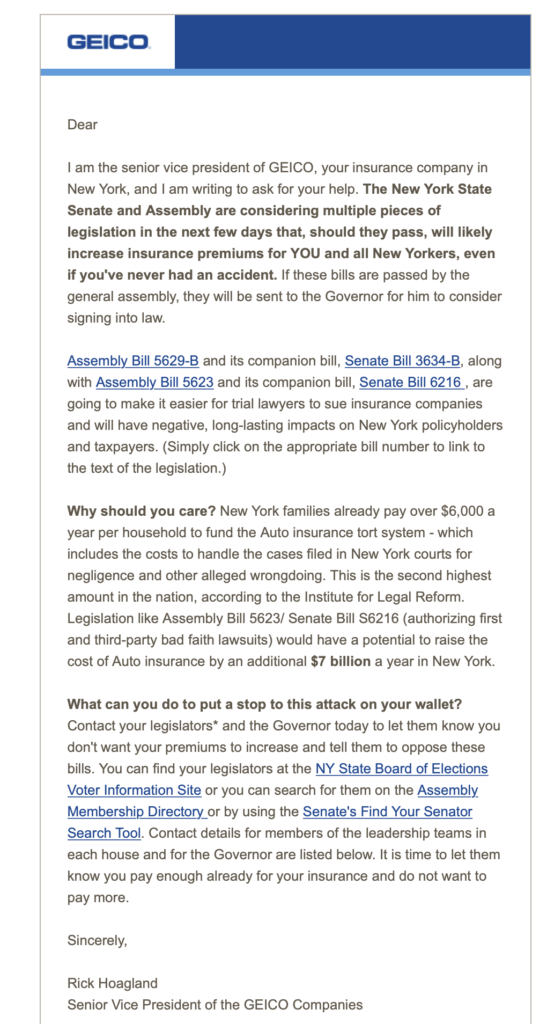
Warren Buffett’s Geico, you will not be surprised to learn, wants immunity from bad faith claims. They want the “free money” to continue.